SUBMANDIBULAR GLAND EXCISION FOR SIALOLITHIASIS IN PEDIATRIC POPULATION
Summary
Although pediatric submandibular sialolithiasis is a rare entity, it should be taken into consideration in pediatric cases with swelling of the neck. Sialolithiasis is the most common cause of the inflammatory diseases of major salivary glands and 87 % of this occurs in submandibular gland. Submandibular gland exicision is the standart treatment for all age groups in case of sialolithiasis. Due to close contiguity, marginal mandibular and hypoglossal nerve paresis, in permanent and temporary manner might be seen. The data of 15 pediatric patients under the age of eighteen-year-old with submandibular sialolithiasis, who underwent gland excision between 2002-2012 in Hacettepe University Department of Otorhinolaryngology, Head and Neck Surgery, were evaluated retrospectively. Medical records were examined for age, gender, symptoms, perioperative and postoperative complications. The age was ranging between 4- 18 years. Submandibular sialolithiasis was detected in the right submandibular gland at 8 patients (53%) and in the left gland at 7 cases (47 %). Submandibular swelling is the most common symptom (60 %). Transient paresis of marginal mandibular branch of facial nerve was the most common complication (33 %). One patient showed transient paresis of hypoglossal nerve. None of the cases had a permanent motor nerve palsy. Except four patients who had preoperative xerostomia, none of the patients complained about postoperative xerostomia. Hematoma formation and seroma did not seen in any of the patients.Introduction
The submandibular gland is located in the submandibular fossa in close relation to neurovascular structures[1]. The submandibular glands are responsible for %70 of resting salivary flow. Normal salivary flow is important for maintaining good oral hygiene. Lack of normal flow predisposes to an increased incidence of dental caries and symptomatic xerostomia[2].Sialolithiasis is the most common cause of inflammatory diseases of large salivary glands and occurs in about 1.2 % of the population mostly in the submandibular gland (87 %). The incidence of sialolithiasis is shown to peak in the third to sixth decade of life. Salivary gland stones are single or multiple, located in the efferent duct distally or proximally, rarely occur intraparenchymally, representing various shapes and sizes[3-5]. Sialolithiasis of the submandibular gland, leading usually to chronic inflammation of this gland, is the most common indication for submandibular gland excision for adult population[6]. Pediatric sialolithiasis is a very rare situation and it should be adressed properly when it causes clinical symptoms.
The patients either adult or pediatric with sialolithiasis of submandibular gland mostly complain of swelling the submandibular gland that can usually be associated with pain with during meals, xerostomia and pus secretion from the Wharton duct[7]. For diagnosis, imaging techniques are required besides the clinical symptoms. Most useful and non-invasive technique is ultrasound(US). Magnetic resonance imaging (MRI) and Computer tomography (CT) are also useful as an diagnostic tool[8]. Invasive therapeutic techniques such as sialoendoscopy also are taken advantage of diagnosis.
Submandibular gland excision is the gold standard treatment for patients with all age groups[9]. In recent years, Sialoendoscopic removal of salivary stone is gaining acceptance if it is located in only the Wharton duct[10]. The aim of this study was the documentation and analyses sialolithiasis occurence, localization and postoperative complication in pediatric population.
Methods
The data of 15 pediatric patients under eighteen with sialolithiasis of the submandibular gland, who underwent transcervical gland exicision between 2002-2012 in the Hacettepe University Department of Otorhinolaryngology, Head and Neck Surgery, were evaluated retrospectively. Patient data were examined for age, gender, symptoms and peri- and postoperative complications. Ultrasound was performed in all cases for preoperative diagnosis. Ct was also used to detect localization of sialolithiasis which could not be detected with US in 2 patients.Results
9 patients (%60) were male with 6 patients female(%40). The age range was 4 to 18. 8 patients (%53) underwent excision of right and 7 patients of left gland(%47). Submandibular swelling is the most seen symptom (%60). 4 patients complained about xerostomia(%26) and 2 patients of pus secretion from wharton canal (%13).Transient paresis of marginal mandibular branch of facial nerve was the most commonly seen complication(%33). One patient showed transient palsy of hypoglossal nerve. No case of a permanent palsy was observed in this study. No patients complained about postoperative xerostomia except four patients who had preoperative xerostomia. There were also no hematoma or seroma were seen.
Pathological diagnosis were sialolithiasis and chronic sialoadenitis due to the saliva stones. In 2 patients (%13), sialolithiasis was located at wharton duct, in 7 patients(%47), saliva stones were located intraparenchymal and rest were located both intraparenchymal and intracanalicular(%40). Demografic characteristics of patients, symptoms, stone localization and complications are summarized at Table 1.
Table 1: Demographic Characteristic of Patients and Postopeartive Findings
Discussion
The most common pathology affecting the salivary glands is sialolithiasis. The pathogenesis of this disease is still unknown. About 99 % of salivary stones are constituted of calcium phosphates[11,12]. Ninety percent of them arise in the submandibular gland, while only %10 are encountered in the parotid gland. Diagnosis of sialolithiasis is based on its clinical presentation and symptomps. Painful, rapidly increasing salivatory colic character is exhibited especially during meal time[13]. This may be related with mechanical obstruction due to the saliva stones. Ultrasound could be utilizied as an diagnostic tool. It is useful to show either ductal or intraparenchymal stones. CT is the most sensitive method for determination of stones. It could show the stone under 2 mm[14] (Fig. 1-2). US was used in all cases and CT was used only 2 patients in our study.
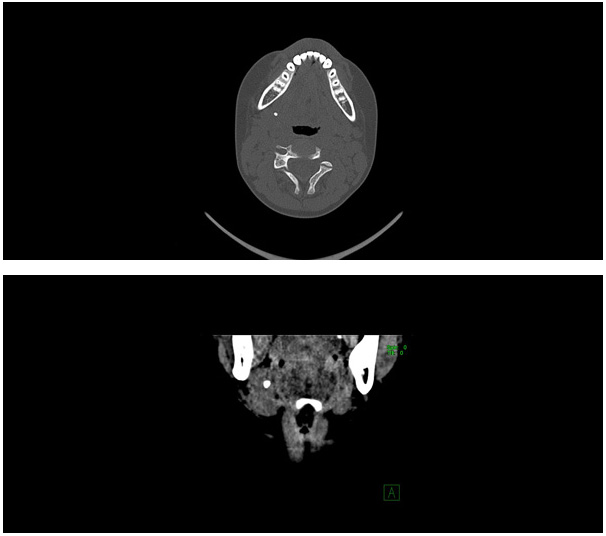 Büyütmek İçin Tıklayın |
Figure 1-2: Right submandibular gland contains intraparenchymal sialolithiasis |
Patients affected by submandibular gland sialolithiasis are presented with a unilateral submandibular swelling, usually associated with pain during meals in cases of sialolithiasis. Other symptoms are xerostomia and pus secretion from the Wharton duct. In our study swelling was the most common symptom, 9cases (%60) showed swelling during the meal time, xerostomia was detected in 4 patiens(%26) and pus secretion was seen 2 in patients (%14)
Sialendoscopy is an interventional procedure allowing diagnosis and simultaneous removal of salivary stones in cases of sialolithiasis, allowing for the preservation of the gland. In a recent study, endoscopy was successful in 97 % of patients with intraductal sialolithiasis of the submandibular gland[15]. Sialoendoscopy is generally performed under local anesthesia then it is diffucult to perform in pediatric patients and successfull rate of sialoendoscopy is too low when the stones localized parenchyme. The disadvantage of this technique is its limited application field, especially at children, since it cannot be used in cases of intraparenchymal sialolithiasis[16].
The lateral transcervical excision (Fig.3) is the standart treatment to the submandibular intraparenchymal sialolithiasis and it should be first choice in pediatric patients owing to limited application field of sialoendoscopy. Nowadays transoral submandibular gland excision was mostly due to the sialolithiasis or chronic sialoadenitis because of salivary stone but it is hardly difficult to perform transoral exicision in pediatric patients because of limited application field and highly complication rate such as saliva fistulas, remnant of the gland, early postoperative submandibular swelling and difficulties of bleeding control[17]. The main advantage of this method is the optimal exposition of the operating field, allowing for the visualization of the involved nerves, minimizing the risk of iatrogenic postoperative complications, especially of the lingual and hypoglossal nerve[18]. It was observed either intraparenchymal (Fig.4-6) or in wharton duct. In this study, we detected salivary stones in 7 patients solely intraparenchymally, it was located only intraductal in 2 patients and the sialolithiasis was detected both intraparenchymally and intraductal in 6 patients.
 Büyütmek İçin Tıklayın |
Figure 3: Submandibular incision |
 Büyütmek İçin Tıklayın |
Figure 4: Revealing the submandibular gland |
 Büyütmek İçin Tıklayın |
Figure 5: Submandibular gland and wharton duct |
 Büyütmek İçin Tıklayın |
Figure 6: Exicised submandibular gland |
This surgery is mostly performed on adult patients. In the literature, pediatric sialolithiasis is a rare disease entity, with fewer than 120 cases having been reported in the literature[19]. We evaluated submandibular gland excision from 15 pediatric patients with sialolithiasis which may be among the largest series of literature. All patients reported the effectiveness of the operation and there were not any reoperations because of retained salivary stones.
Unilateral submandibular gland excision results in a decreased rate of resting salivary flow and might cause xerostomia. It is commonly reported after submandibular gland excision. Springborg, L.K. et all found that %22.1 of the patients complained about xerostomia after surgery[20]. In our study, no patients complained about postoperative xerostomia except four patients who had preoperative xerostomia. Their complaints continued after the surgery.
The main disadvantages of transcervical exicision are the presence of an external scar and the higher rates of marginal mandibular nerve trauma in comparison to other techniques[21]. The marginal mandibular nerve passes superficially to the fascia of the submandibular gland and deeply to the plane of the platysma (Fig.7). Consequently, surgical dissection within the fascia poses the least risk of damage to the nerve[22]. We found an 33% risk of temporary marginal paresis and one patient showed temporary hypoglossal nerve paresis. This rate is relatively higher than other studies in literature . Mentioned above studies mostly include adult patients and we don't have large series pediatric sialolithiasis. Submandibular gland exicision in pediatric patients should be performed with small incision because of wound healing. This reason may be cause slightly higher marginal paresis rate but it is transient not permanent.
In the literature, postoperative hematoma rate was approximately %10 at adult age. Kukuckova, B. et al found that a significantly higher risk of hematomas in patients with sialoadenitis compared to sialolithiasis[23]. We did'nt observe any hematoma or seroma. This can be related with all patients who are pediatric and with sialolithiasis in this study. Similarly, postoperative infection was not detected any patients in this study. There is no knowledge about sialolithiasis rate when it comes to postoperative complication in pediatric population.
Conclusion
Although submandibular sialolithiasis is a rare diseases entity, swelling of the neck in pediatric patients should be considered as an submandibular sialolithiasis. Treatment options of sialolithiasis in pediatric patients differs in as against an adult patients. Gold standart treatment is transcervical exicision. In pediatric patients, this surgery can be hazardous with regard to high rate of complication. Thus, surgeon should be carefull during surgery in pediatric patients with sialolithiasis.Reference
1) Hald, J. and U.K. Andreassen, Submandibular gland excision: short- and long-term complications. ORL J Otorhinolaryngol Relat Spec, 1994. 56(2): p. 87-91.
2) Rallis, G., C. Mourouzis, and N. Zachariades, A study of 55 submandibular salivary gland excisions. Gen Dent, 2004. 52(5): p. 420-3. [ Özet ]
3) Preuss, S.F., et al., Submandibular gland excision: 15 years of experience. J Oral Maxillofac Surg, 2007. 65(5): p. 953-7. [ Özet ]
4) Torroni, A.A., et al., Transcervical submandibular sialoadenectomy. J Craniofac Surg, 2007. 18(3): p. 613-21. [ Özet ]
5) Marchal, F. and P. Dulguerov, Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg, 2003. 129(9): p. 951-6. [ Özet ]
6) Iro, H., J. Dlugaiczyk, and J. Zenk, Current concepts in diagnosis and treatment of sialolithiasis. Br J Hosp Med (Lond), 2006. 67(1): p. 24-8. [ Özet ]
7) Goh, Y.H. and D.S. Sethi, Submandibular gland excision: a five-year review. J Laryngol Otol, 1998. 112(3): p. 269-73. [ Özet ]
8) Lee, Y.Y., et al., Imaging of salivary gland tumours. Eur J Radiol, 2008. 66(3): p. 419-36. [ Özet ]
9) Hernando, M., et al., Surgical complications of submandibular gland excision. Acta Otorrinolaringol Esp, 2012. 63(1): p. 42-6. [ Özet ]
10) Zenk, J., et al., Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg, 2012. 147(5): p. 858-63. [ Özet ]
11) Huoh, K.C. and D.W. Eisele, Etiologic factors in sialolithiasis. Otolaryngol Head Neck Surg, 2011. 145(6): p. 935-9. [ Özet ]
12) Sabot, J.F., et al., Analytical investigation of salivary calculi, by mid-infrared spectroscopy. Analyst, 2012. 137(9): p. 2095-100. [ Özet ]
13) Beahm, D.D., et al., Surgical approaches to the submandibular gland: a review of literature. Int J Surg, 2009. 7(6): p. 503-9. [ Özet ]
14) Kopec, T., M. Wierzbicka, and W. Szyfter, [A proposal for the classification of chronic sialadenitis of the major salivary glands with current diagnostic and treatment schedule]. Otolaryngol Pol, 2011. 65(3): p. 188-93. [ Özet ]
15) Ziegler, C.M., et al., Endoscopy: a minimally invasive procedure for diagnosis and treatment of diseases of the salivary glands. Six years of practical experience. Br J Oral Maxillofac Surg, 2004. 42(1): p. 1-7. [ Özet ]
16) Chang, Y.N., et al., Comparison of the intraoral and transcervical approach in submandibular gland excision. Eur Arch Otorhinolaryngol, 2013. 270(2): p. 669-74. [ Özet ]
17) Winkel, R., et al., [Surgical results of submandibular gland excision]. Ugeskr Laeger, 2000. 162(40): p. 5354-7. [ Özet ]
18) Biffoni, M., et al., [Submandibulectomy in the treatment of pathology of the submandibular gland: our experience 1970-1995]. G Chir, 1997. 18(10): p. 477-80. [ Özet ]
19) Nahlieli, O., et al., Pediatric sialolithiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2000. 90(6): p. 709-12. [ Özet ]
20) Springborg, L.K. and M.N. Moller, Submandibular gland excision: long-term clinical outcome in 139 patients operated in a single institution. Eur Arch Otorhinolaryngol, 2013. 270(4): p. 1441-6. [ Özet ]
21) Hong, K.H. and Y.K. Kim, Intraoral removal of the submandibular gland: a new surgical approach. Otolaryngol Head Neck Surg, 2000. 122(6): p. 798-802. [ Özet ]
22) Moller, M.N. and C.H. Sorensen, Risk of marginal mandibular nerve injury in neck dissection. Eur Arch Otorhinolaryngol, 2012. 269(2): p. 601-5. [ Özet ]
23) Kukuckova, B. and M. Svec, Surgical management of submandibulary gland diseases: ten years of experience. Bratisl Lek Listy, 2011. 112(5): p. 264-8. [ Özet ]




